What Causes Skin Cancer?
While UV radiation from the sun is the most common cause of skin cancer, there are others! Genetics, viruses (HPV, Merkel cell polyomavirus), trauma, ionizing radiation, indoor tanning, immunosuppression, certain medications, tobacco use, chronic scarring and inflammatory conditions, and chemicals (arsenic, coal tar, soot, mineral oil, nitrogen mustard, polychlorinated biphenyls, mineral oil, pesticides) may also cause skin cancers.
Types of Skin Cancer
-
Basal Cell Carcinoma
1 in 5 Americans will develop a skin cancer in their lifetime, and basal cell carcinoma is by far the most common type of skin cancer. It is slow growing and primarily locally destructive. First, the cancer destroys skin, then progresses to destroy deeper structures including bone. Basal cell carcinoma is typically not life threatening, but left untreated up to 1 in 1,000 will metastasize (spread to other parts of the body).
-
Squamous Cell Carcinoma
Squamous cell carcinoma is the second most common type of skin cancer. It may grow rapidly or slowly. Squamous cell carcinoma is typically not life threatening when treated in a timely manner. However, left untreated it has a 1-5% risk of metastasizing (spreading to other parts of the body).
-
Melanoma
Melanoma is the third most common type of skin cancer. It accounts for 4% of all skin cancers. It can be more aggressive than basal cell and squamous cell carcinomas, with a higher risk of spreading to other parts of the body (metastasizing) left untreated. In addition to surgical removal, your dermatologist may recommend additional workup and treatment depending on the stage of the melanoma at diagnosis.
Less Common Skin Cancers
Prognosis and treatment depends on tumor type and characteristics. Your dermatologist and surgeon will formulate the best treatment plan for you.

Dermatofibrosarcoma Protuberans
- Atypical Fibroxanthoma
- Angiosarcoma
- Dermatofibrosarcoma Protuberans
- Extramammary Paget’s Disease
- Kaposi’s Sarcoma
- Merkel Cell Carcinoma
- Microcystic Adnexal Carcinoma
- Mucinous Carcinoma
- Other Eccrine Carcinomas
- Pleomorphic Dermal Sarcoma
- Sebaceous Carcinoma
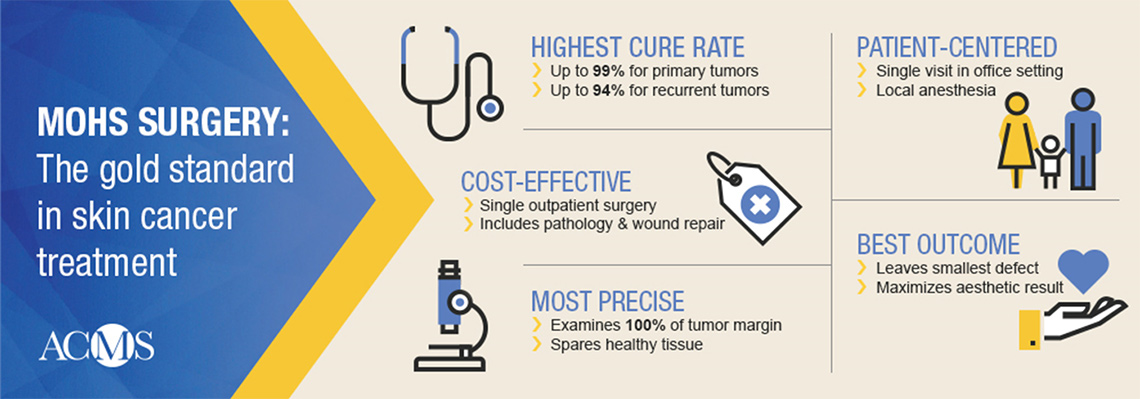
What is Mohs Micrographic Surgery?

Why did your dermatologist choose Mohs Micrographic Surgery for your skin cancer treatment?
Reconstructive surgery following Mohs Micrographic Surgery
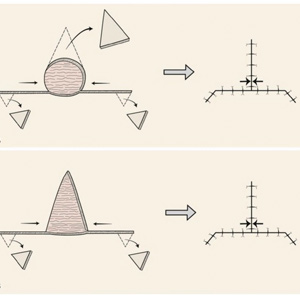
After skin cancer is treated surgically, the wound is most often repaired on the same day by your skin cancer surgeon. Wounds are closed under local anesthesia. The wound may be closed in a straight line (also known as primary closure), with a flap (transfer of adjacent skin), or with a graft (transfer of distant skin and sometimes structural cartilage). There are innumerable subtypes of these repairs. In some cases the wound is left to heal on its own (sometimes with the help of special wound dressings or skin substitutes) in a process called second intention healing. Your surgeon will choose the repair that maintains function, optimizes appearance, and satisfies patient preferences.
Pre & Post-Operative Information
Before Mohs Micrographic Surgery
Checking in: Arrive at 9303 Pinecroft, Suite 160, The Woodlands, Texas 77380 10 minutes before your assigned time.
What to expect: On the day of surgery, you will be given local anesthesia only. We inject the anesthesia directly into the affected area so that patients experience no pain after the anesthetic takes effect. The procedure takes 30 minutes to 1 hour, depending on the size and depth of the skin excision. Patients remain awake and fully informed during their excision. Once the excision is performed, the lesion is placed in a specimen container and sent to the pathologist for evaluation. The dermatopathologist checks the margins or gives us a diagnosis if necessary.
Medications: Please take all your normal medications, including blood thinners, on the day of your surgery.
Antibiotics: If you usually require antibiotics prior to dental work, please let the nurse know when you arrive at your appointment. Medical conditions that sometimes require preoperative antibiotics include artificial heart valves, heart murmurs, artificial joints, and related problems.
Special occasions: Surgery often creates swelling and bruising. The post-op dressing may be rather large and obvious. Please keep this in mind as you arrange your social/work schedule and consider any important events you may have already planned.
Activity limits after surgery: It’s important to know the physical limitations following your excision. Do not engage in strenuous physical activity or submerge in pools or lakes after your surgery. These limitations are likely to impact golf, tennis, gym activities, etc. Depending on the anatomical site, some physical activity is allowed. Ask your doctor specifically what you can and can’t do (including travel plans), and they will explain the physical limitations necessary for your healing.
Transportation: Skin surgery (excision) is done under local anesthesia. Most patients are able to drive themselves home after the surgery. However, if you’ve had problems after procedures you’ve had done in the past, it may be advisable to bring a companion with you on the day of your surgery to drive you and make sure you get home safely after your surgery. If your surgery is near the eye, postoperative bandaging can also be interference, and having someone drive you to and from
The Day of Mohs Micrographic Surgery
Checking in: Arrive at 9303 Pinecroft, Suite 160, The Woodlands, Texas 77380 10 minutes before your assigned time.
What to expect: On the day of surgery, you will be given local anesthesia only (similar to what was given to you during your initial biopsy). You will remain awake. You will verify the location of the skin cancer prior to the onset of the surgery. Once the area is numb, the tissue containing the skin cancer will be removed, taking a small safety margin. The first layer (“Stage I”) will be processed in our laboratory. The wound will be treated for bleeding, and a bandage will be placed to keep you comfortable while you wait approximately 45 minutes-1 hour (for the processing of the tissue). The surgeon will examine the pathology in the lab, checking all the margins.
If any margin is not clear, a second layer (“Stage 2”) will be taken. The area will be re-anesthetized, and the surgeon will remove more skin only in the area where cancer exists. This process will continue until all the skin cancer is removed. Unfortunately, there is no method to predict how many layers or stages will be taken. Once the margins are cleared, the surgeon will discuss the best ways to close the defect. Most wounds may be closed with stitches. A larger wound may require a skin graft or a flap.
Medications: Please take all your normal medications, including blood thinners, the morning of your surgery. If you are a diabetic, please bring your insulin or medications with you, as well as a snack to avoid having low blood sugar during your day with us.
Antibiotics – If you usually require antibiotics prior to dental work, please let the nurse know when you arrive at your appointment. Medical conditions that sometimes require preoperative antibiotics include artificial heart valves, heart murmurs, artificial joints, and related problems.
What to bring with you on the day of your surgery
- Bring snacks – Since you could be at the office for an extended time, you may bring snacks and/or lunch with you.
- Bring a sweater – Bring a sweater or jacket that buttons or zips down the front and will not disturb your wound dressing during removal.
- Bring something to do – You will be spending much of the day in our office. There will be 45-60 minute waiting periods between layers/stages, so it is nice to have something to keep you occupied, such as books, magazines, knitting, music, or work.
Planning ahead:
- Other appointments – It is important to realize that no matter how small the skin cancer appears to be, looks can be deceiving. Since your surgery may last the entire day, you should not schedule any other appointments that day.
- Special occasions – Surgery often creates swelling and bruising. Also, the post-op dressing may be rather large and obvious. Keep this in mind as you arrange your social/work schedule. If an important event is already planned.
- Activity limits after surgery – If surgery was performed on your face, we recommend that you keep your activity level to a minimum for 2-3 days (the blood pressure elevation related to exercise can lead to bleeding). If you have stitches in an area that will be under tension or significant movement (neck, back, arms, legs), you will need to avoid heavy lifting (anything over 5 pounds) or exercise for at least 2 weeks and possibly longer. We also advise that you limit out-of-town travel for the first 7 days after surgery. You should also wait at least 7 days before going into a pool or the ocean. If surgery is around your mouth area, you may need to eat soft foods, such as soup, milkshakes, or yogurt, for 48 hours.
- Transportation – Mohs surgery is done under local anesthesia. Most patients are able to drive themselves home after the surgery. However, if you’ve had problems after procedures you’ve had done in the past, it may be advisable to bring a companion with you on the day of your surgery to drive you and make sure you get home safely after your surgery. If your surgery is near the eye, postoperative bandaging can also be interference, and having someone drive you to and from surgery should be considered.
- Rescheduling – If you need to reschedule your surgery, please notify the office as soon as possible.
After Mohs Micrographic Surgery
After Surgery Wound Care Instructions (unless otherwise instructed at the time of surgery)
Supplies
- You will need to have hydrogen peroxide, Q-tips or cotton balls, Vaseline or Aquaphor (unless a substitute antibiotic ointment is given), and an appropriate-sized bandage.
Wound care
- Dressing needs to be kept dry for 24 hours. Afterwards, remove all bandaging to expose sutures. The wound may then get wet in the shower and may be gently patted dry. No scrubbing. You may let soap and water run over the surgery site.
- After the bandage is removed, clean the wound once daily with hydrogen peroxide. You may use Q-tips, cotton balls, or pour the hydrogen peroxide over the wound. Remove all crusted material that comes off easily.
- Dry the area and apply a liberal amount of Vaseline or Aquaphor twice daily.
- Cover your wound with an appropriate-sized bandage. You may need to trim a larger bandage to fit.
- Continue wound care until sutures are removed.
Pain control
- Unless your doctor states otherwise or gives you a prescription for pain medication, take Tylenol for pain as needed. Avoid Motrin, Aleve, and Ibuprofen as these have blood-thinning properties and may cause bleeding.
- Avoid activity that causes swelling. Swelling can cause significant pain.
- Use an ice pack numerous times over the first 48 hours. Apply an ice pack for 20 minutes at a time, with approximately 2 hours between sessions. (Hint: Frozen peas in a zip lock bag work very nicely.)
Activities
- After surgery, go home and take it easy (no exertion, lifting, bending, or straining). Exertional activity may cause pain, bleeding, infection, and a poor cosmetic outcome.
- Do not do any heavy lifting or work out exercising for at least: [ ] 1 week [ ] 10 days [ ] 2 weeks
- Do not submerge wound area in any type of dirty water (i.e.: no lakes, pools, oceans, or hot tubs).
For facial wounds
- Keep your head elevated above your heart while resting and sleeping.
- It is normal to have bruising or discoloration around or below the surgery site, especially around the eyes. Do not be alarmed; this will fade with time.
Notify the doctor if the following occurs:
- Bleeding that saturates your dressing (spotting on the dressing is expected). To stop bleeding, hold direct pressureover the dressing for 20 minutes with gauze or a thin towel. Do not remove the dressing. The pressure must be constant for 20 minutes – do not remove pressure to check if the bleeding has stopped for a full 20 minutes.
- Temperature greater than 100°F, severe nausea or vomiting, severe pain not relieved with Tylenol and ice packs.
- Signs of infection (i.e.: worsening redness, swelling, foul-smelling drainage, pain or heat).
For questions or concerns, call the surgery center:
- (Monday-Friday 8:30AM-4:30PM) , ext. 166, 162, 163, 155
- If you need to reschedule your surgery, please notify the office as soon as possible.
-
Activity Restrictions
Video created by the American College of Mohs Surgery -
Post Operative Diet
Video created by the American College of Mohs Surgery -
Post Operative Pain
Video created by the American College of Mohs Surgery -
Swelling, Bruising, and Bleeding
Video created by the American College of Mohs Surgery -
Dressing Changes
Video created by the American College of Mohs Surgery -
Other General Wound Care Measures
Video created by the American College of Mohs Surgery -
Skin Cancer Prevention
Video created by the American College of Mohs Surgery -
Long Term Wound Healing
Video created by the American College of Mohs Surgery
Photo Gallery
* The following images contain graphic surgical content. Viewer discretion advised. Patient consent obtained for use of de-identified images for educational purposes.
Mohs Micrographic Surgery, Skin Cancer Surgery, and Reconstructive Surgery
Face
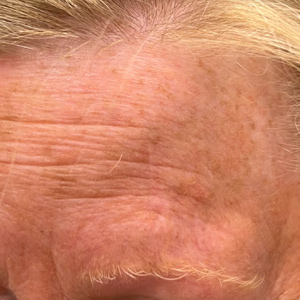
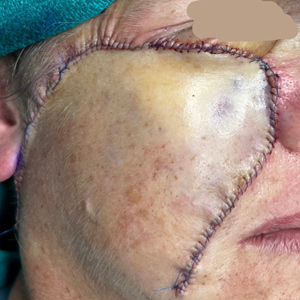
Case 1
Mohs Micrographic Surgery on the forehead + reconstructive surgery with a flap + 1 week post-op photo. The scar will become less red and puffy with time.
Case 2
Mohs Micrographic Surgery on the cheek + reconstructive surgery with a straight line closure + 3 month post-op photo. The scar will become even more subtle time.
Case 3
Mohs micrographic surgery on the cheek + reconstructive surgery with a linear closure + 1 week post-op + 12 month post-op photos
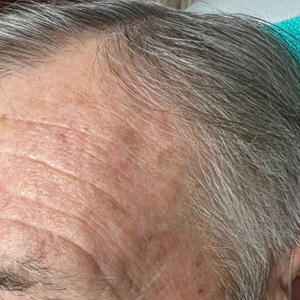
Case 4
Mohs micrographic surgery on the forehead + reconstructive surgery with a flap + 12 month post-op photos
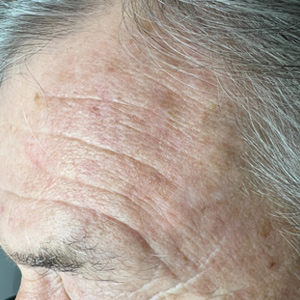
Case 5
Mohs micrographic surgery on the forehead + reconstructive surgery with a linear closure + 1 week post-op + 6 month post-op photos
Case 6
Mohs micrographic surgery on the forehead + reconstructive surgery with a flap + 6 month post-op photos
Case 7
Mohs micrographic surgery on the cheek + reconstructive surgery with a flap
Case 8
Mohs micrographic surgery on the nasal crease + reconstructive surgery with a linear closure + 12 month post-op photo
Scalp
Case 1
Skin cancer excision + reconstructive surgery with a flap + 2 week post-op photo. The scar will become less red and puffy with time.
Neck
Case 1
Mohs Micrographic Surgery on the ear and neck + reconstructive surgery with straight line closures + 10 month post-op photos.
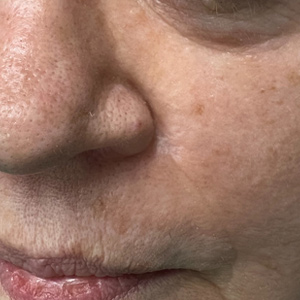
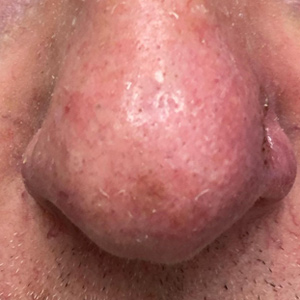
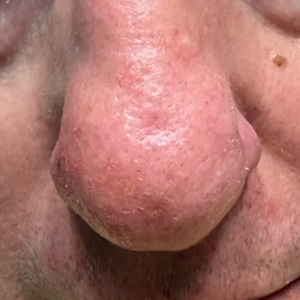
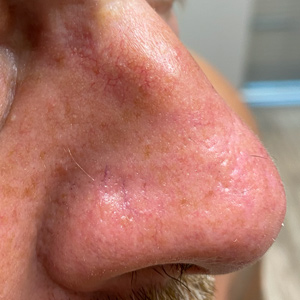
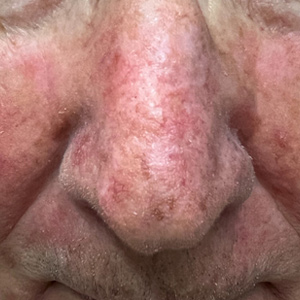
Nose
Case 1
Mohs Micrographic Surgery on the Nose + reconstructive surgery with a flap + 1 week post-op + 4 month post-op photos
Case 2
Mohs Micrographic Surgery on the nose + reconstructive surgery with a straight line closure + 1 week post-op photo + 2 month post-op photo.
Case 3
Mohs micrographic surgery on the nose + reconstructive surgery with a full thickness skin graft + 1 week post-op + 12 month post-op photos
Ears
Case 1
Mohs Micrographic Surgery on the ear + reconstructive surgery with a flap + 2 week post-op photos. The scar will become less red and puffy with time.
Case 2
Mohs Micrographic Surgery on the ear and neck + reconstructive surgery with straight line closures + 10 month post-op photos.
* Patient consent obtained for use of de-identified images for educational purposes.
Case 3
Mohs micrographic surgery on the ear + reconstructive surgery with a linear closure + 1 week post-op + 9 month post-op photos